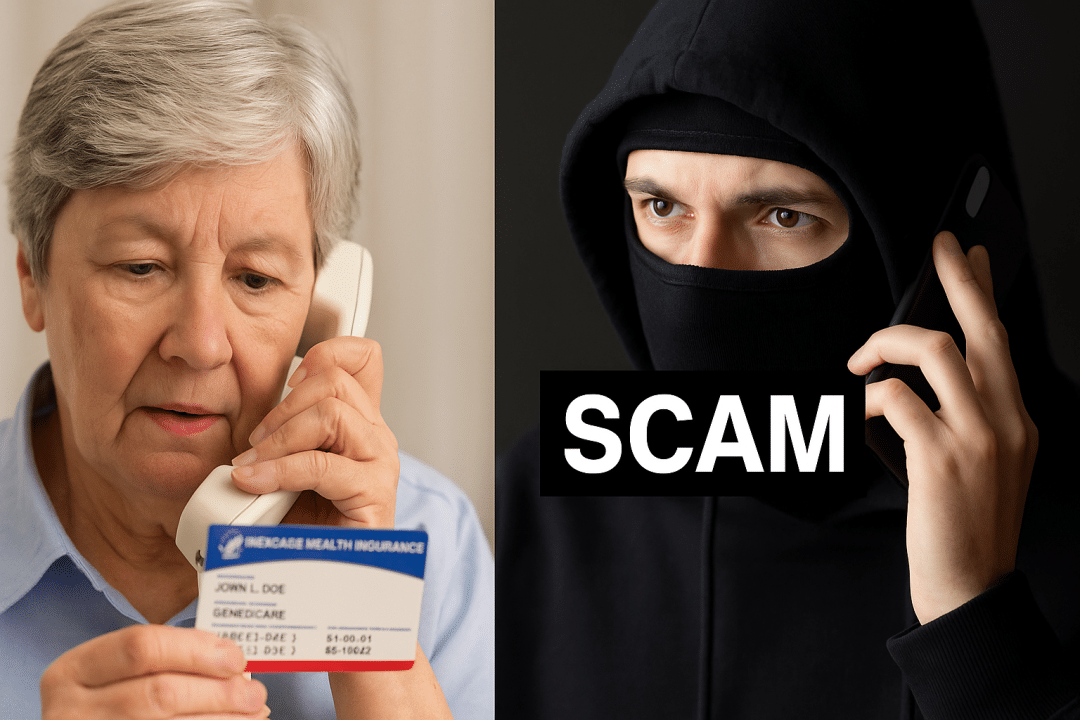
As Medicare Fraud Prevention Week unfolds, federal and local investigations have uncovered alarming trends in how fraudsters are exploiting the Medicare system. With schemes costing U.S. taxpayers an estimated $60 billion annually, experts say older adults must stay vigilant.
Fraud tactics hitting Indiana and beyond
In Indiana, WRTV Investigates revealed a wave of fraudulent Medicare activity, including:
- Unordered genetic testing kits
- Phantom billing for durable medical equipment (DME)
- Remote patient monitoring claims
- Catheter scams totaling over $3,000 per individual
Nancy Moore, director of the Indiana Senior Medicare Patrol, warns that stolen Medicare numbers are traded on the dark web and used to file false claims. “Medicare numbers are more valuable than Social Security numbers,” she said.
National cases highlight massive fraud
Recent prosecutions emphasize the scale of the problem:
- A North Carolina man laundered $3 million as part of a $100 million DME scam.
- Two Texas residents were charged with filing $359 million in fraudulent genetic testing claims.
These cases highlight how widespread and organized Medicare fraud has become.
Common signs of a Medicare scam
Experts advise looking out for these red flags:
- Promises of free medical equipment or testing not ordered by your doctor
- Calls claiming you’re preapproved for new plans or refunds
- Requests to verify or update your Medicare card
- Threats to cancel your benefits if you don’t act immediately
How to protect yourself
To guard against scams:
- Never share your Medicare number unless with a verified provider
- Don’t trust caller ID—scammers can spoof government numbers
- Avoid clicking suspicious email links
- Shred old Medicare cards
- Monitor your Medicare Summary Notice or EOB for unauthorized charges
How to report Medicare fraud
Report suspicious activity to:
- Medicare: 1-800-MEDICARE (800-633-4227)
- Senior Medicare Patrol: 1-877-808-2468
- HHS Fraud Hotline: 1-800-HHS-TIPS
- FTC: ReportFraud.ftc.gov
What happens next
CMS has responded with aggressive actions, including halting payments to shady providers, removing convicted individuals from Medicare, and reviewing high-risk claims before payment.
But Moore says vigilance starts with beneficiaries: “Even if you don’t owe anything, false claims hurt everyone by driving up costs.”
Stay protected and informed. Subscribe to our newsletter for updates on Medicare and senior safety.
